Research show people using antidepressants have problems withdrawing from the drugs due to doctors not knowing how to do it correctly, and that it can take months and years due to severe withdrawal effects. Adverse withdrawal effects often are not recognized or misdiagnosed as relapse.
Millions affected
When the SSRI antidepressants first appeared on the market they were presented as drugs that could solve life situations and with no problems related to them. In fact, manufacturers distributed numerous papers with description of withdrawal symptoms from the drugs as being “brief and mild”, based on studies conducted by the drug companies themselves which focused on people who had been on the antidepressants for only 8 to 12 weeks. The result has been that over the years both doctors and the general population have come to believe these drugs can not cause severe and long-lasting withdrawal symptoms on stopping them. And further that stopping the use of these drugs following a treatment would not be a problem.
What has not been the focus in research is that the longer people are on these antidepressants, the harder it is to stop and the more severe the withdrawal effects.
Research presented at this year’s European Psychiatric Congress show there are major problems related to this and research indicate that more than half will have problems stopping, amounting to millions in Europe being affected.
Antidepressants cause residual change to cell structure
The use of antidepressants causes changes to the body and its ability to regulate the use of its own neurotransmitters used to control numerous bodily functions. The result of this change of the cell structures is that once a user has stopped the antidepressants this can cause withdrawal effects and these can last months or years after the drug has left the system. The new research explain what many users have said they have felt for years.
Dr Mark Horowitz, an expert and Clinical Research Fellow in Psychiatry at the National Health Service (NHS) in England, presented extensive research findings that put a new light to the problem.
“When you stop the drug, let’s say months or years after the patient had been started on drug treatment following a stressful period in their life, the antidepressant is metabolized by the liver and kidneys in a few days or weeks. But what doesn’t change in a few days or weeks is the residual changes to the post-synaptic serotonin receptors and other systems downstream of this,” Dr. Horowitz told.
In studies on humans, there are changes to the serotonergic system that persists for up to four years after the antidepressants are stopped.
“In other words, you now have a system that is less sensitive to serotonin being exposed to normal levels of serotonin after the drug is removed. And overall, this could be seen as a low serotonin syndrome,” he clarified.
This of course is a very simplified version of what’s going on. There are many other neurotransmitters and downstream effects of these changes that may also persist for long periods after the drug is stopped. All of these changes also are likely to explain the wide-ranging and long-lasting symptoms that occur after stopping antidepressants.
Adaptation to the drug
The underlying problem that has often been neglected is that years of use has caused an adaptation to the antidepressant drug by the body and brain and this condition persists for longer than it takes the drug to be eliminated from the body, and that’s what causes withdrawal effects.
Dr Mark Horowitz explains why withdrawal effects last for more than a few days or weeks after the drug is out of the system, “it’s not the time taken for the drug to leave the system that determines the length of the effect. It’s the time taken for the system to readapt to the drug not being there that explains how long withdrawal symptoms can last for.”
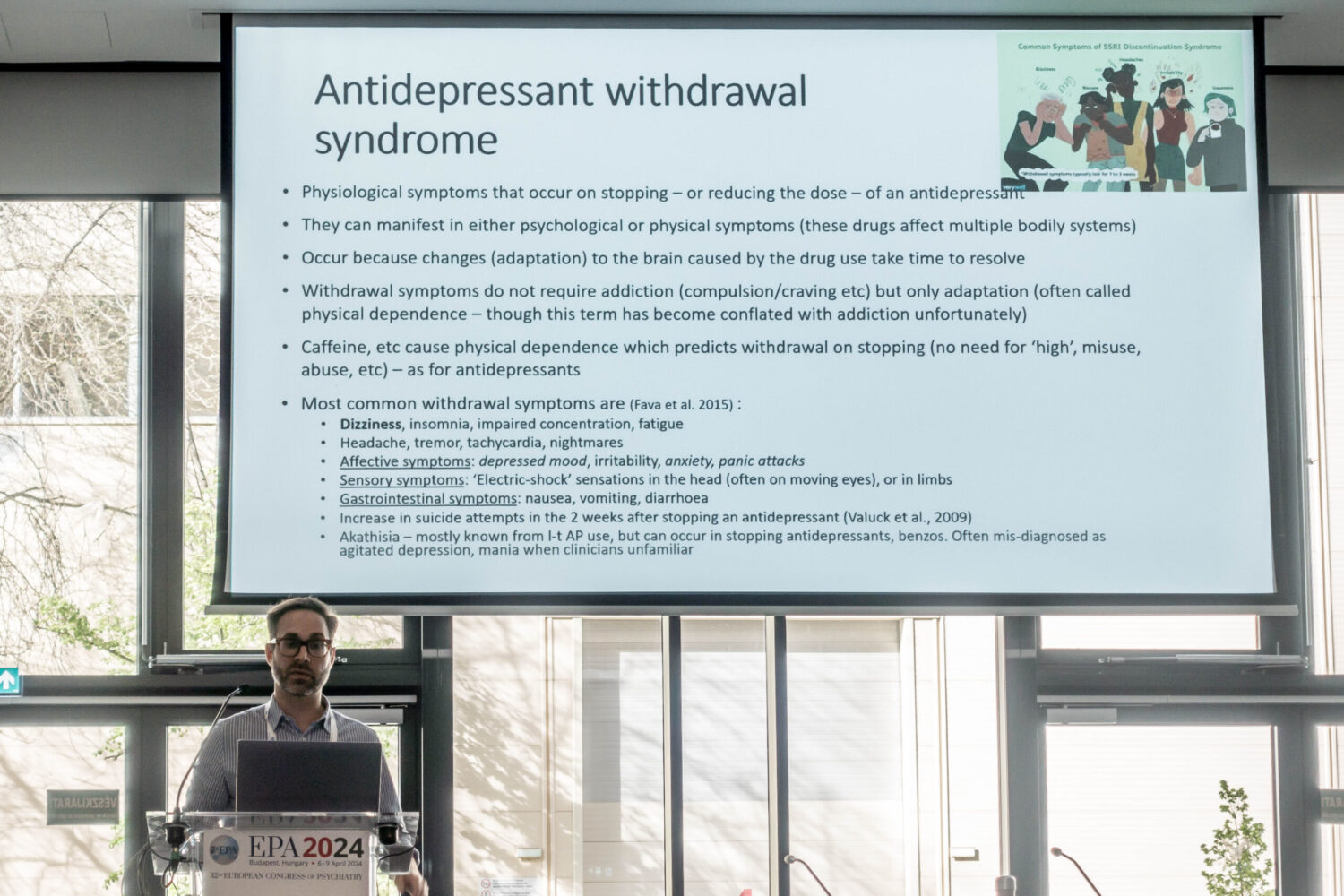
Antidepressant withdrawal syndrome is a set of physiological symptoms that occur on stopping or reducing the dose of an antidepressant. They can manifest in either psychological or physical symptoms because these drugs affect so many bodily systems. They occur because adaptations to the brain caused by the drug take time to resolve.
Dr Mark Horowitz pointed out that it’s important to understand that withdrawal symptoms do not require addiction, all that is required is adaptation to the drug. This is often referred to as physical dependence. Physical dependence in pharmacological terms means the process of adaptation to appear to exposure to a drug that affects the brain, which is true for antidepressants (and, for example, to caffeine, which does not generally cause addiction but can cause physical dependence and therefore withdrawal effects).
As the SSRI antidepressants act on a neurotransmitter mechanism that influence not only mood but many bodily systems withdrawing from the drug after years of adaptation thus can cause strong reactions on many of these functions and their influence on one’s life.
Symptoms of withdrawal
There are dozens and dozens of possible effects that can be caused. Symptoms include dizziness, insomnia, impaired concentration, fatigue, headache, tremor, tachycardia, and nightmares. Withdrawal can even cause affective symptoms such as depressed mood, irritability, anxiety, and panic attacks.
“We know that these are symptoms of withdrawal and not just relapse (a return of someone’s underlying condition), because they have been found in studies of people who stopped antidepressants with no underlying mental health conditions,” Dr Mark Horowitz told. He mentioned examples such as people who are given these drugs for pain, for the menopause, and even in healthy volunteers.
There are other effects including an increase in suicide attempts in the two weeks after stopping antidepressants. It has been attributed to withdrawal effects itself because it’s too quick for relapse to explain this increase in symptoms. Dr Mark Horowitz further noted that they have also found in studies that while 30% of those who responded were suicidal before starting medication, 60% became suicidal after stopping so that this means for 30% of people they will experience being suicidal for the first time in their lives because of withdrawal effects.
The maybe most disturbing symptom from withdrawal of antidepressants, which often has been neglected, is a condition known as akathisia. Akathisia is a movement disorder usually caused by a psychoactive substance in which the individual generally will experience an intense sensation of unease or an inner restlessness that often prompts the patient to pace backwards and forwards and can be an intensely unpleasant experience. Dr Mark Horowitz noted that it is often recognised as a long-term consequence of antipsychotic exposure, but withdrawal from antidepressants and benzodiazepines and a variety of other psychiatric drugs can also cause the condition.
“It is the most horrible presentations that I see. People are pacing, they feel agitated, they feel terror. A lot of them are talking about suicide because it is a state in which you get no rest and no calm, often for weeks and sometimes longer,” Dr Mark Horowitz pointed out.
And it’s important as this condition is often misdiagnosed when people are presented to the emergency department as agitated depression, as mania, because many clinicians and others are unfamiliar with the fact that coming off these drugs can cause akathisia.
Withdrawal effects not recognized or misdiagnosed as relapse
Tens of thousands users of antidepressants from Europe every month are seeking information and advice from American peer support forums on how to come off their medications. Their stories are for many very similar.
The research group of Dr Mark Horowitz surveyed 1,300 of these. Three quarters of them said their doctor’s advice on withdrawing was unhelpful.
The major reasons where that the doctor had recommended a rate of reduction that was much too quick. And that the treating doctors weren’t familiar enough with withdrawal symptoms to have any advice, or they told the user that stopping with antidepressants would not cause withdrawal symptoms.
Dr Mark Horowitz indicated that doctors often still believe that withdrawal effects from antidepressants are “brief and mild”. And they do not know that withdrawal symptoms include anxiety, depressed mood, and insomnia.
“It’s easy to confuse with a relapse of depression or anxiety, especially when it’s in the clinician’s minds that withdrawal effects are brief and mild. Someone turns up with severe symptoms that are long lasting, it’s very hard to put the connection together,” Dr Mark Horowitz added.
Another disturbing fact is that withdrawal effects is not only related to antidepressants. “The same is true for coming off of all psychiatric drugs. Often the changes produced on the brain by psychiatric drugs can persist for months or years after stopping, which is why withdrawal syndromes can last a lot longer if it takes the drug to be eliminated from the body,” Dr Mark Horowitz pointed out.