The recent report published by the High Council for Family, Childhood and Age (HCFEA) warns of the psychological suffering of children and adolescents, as well as the chronic lack of resources allocated to care, education and social intervention in mental health in France. In our previous article we detailed the continuous and inappropriate increase in the consumption of psychotropic drugs in the paediatric population in France.
Here we analyse the old idea that a mental disorder can be caused by a brain abnormality. And that, being of biological origin, this dysfunction can be solved by chemical, electrical or mechanical treatment. This approach has been favoured for a long time, but the results remain limited. Because, in fact, anomalies are ‘associated’ with mental disorders… the problem is their causality.
These prescriptions, often outside of international scientific consensus and regulatory mechanisms (marketing authorizations and recommendations of health agencies), contradict the words of the WHO, which warned, as recently as 2022, that “all over the world […] current practices place psychotropic drugs at the center of the therapeutic response, whereas psychosocial and psychological interventions and peer support are also avenues to be explored and should be offered”.
The international organisation takes a strong stance on the subject, stating that “to succeed in defining an integrated, person-centred, recovery-oriented and rights-based approach to mental health, countries must change and open up mentalities, correct stigmatising attitudes and eliminate coercive practices”. For this to happen, she adds, “it is essential that mental health systems and services broaden their horizons beyond the biomedical model”.
The dead ends of biological psychiatry
Biological psychiatry’ is the direct transcription of this biomedical paradigm.
This approach is based on a biological conception of psychological suffering: it seeks markers (mainly neurobiological and genetic) likely to provide a basis for psychiatric diagnoses and to open the way to essentially medicinal treatments. The UN organisation recalls that it has “dominated mental health research […] in recent decades”. Research, but also French policies over the last twenty years.
If international health institutions deplore the invasion of biomedical approaches, particularly in children, and their consequences in terms of overprescription of psychotropic drugs, it is not because of dogmatism. It is because an updated review of the results of research shows, experimentally and empirically, the impasses of the models inspired by biological psychiatry.
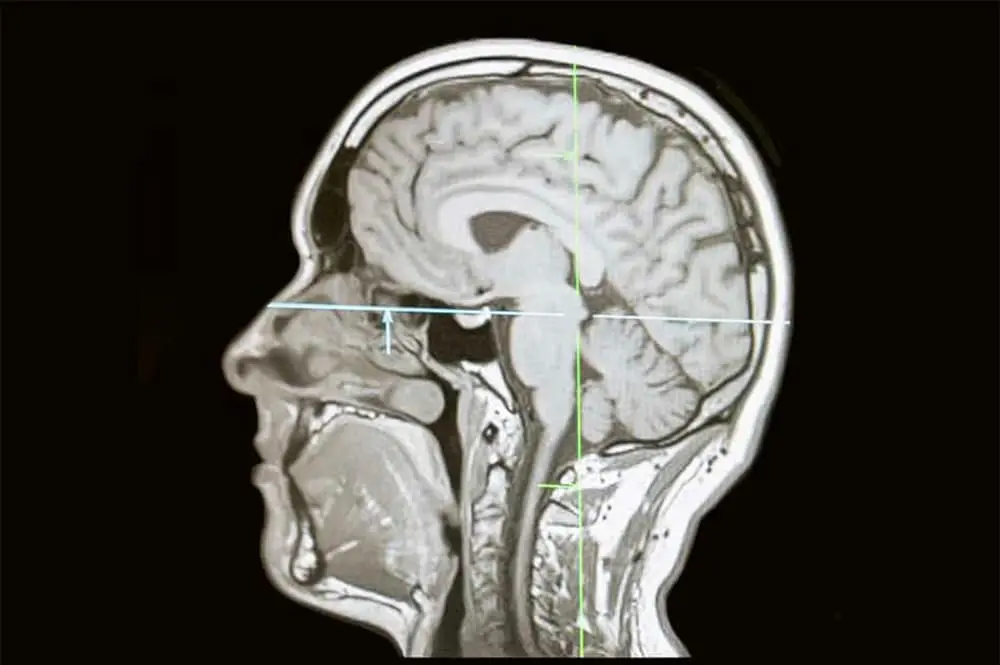
Work on the neurobiology and genetics of mental disorders has increased exponentially over the last forty years, supported by improvements in brain imaging and genetic sequencing technologies. Two main directions have been explored: the search for an organic causality of mental disorders on the one hand, and the development of drug treatments on the other.
Unfortunately, their contributions to clinical psychiatry remain limited and contradictory.
Almost all research hypotheses on the neurological and genetic causes of mental disorders – a fortiori in children – have been refuted by the so-called princeps (reference) studies and subsequent meta-analyses. At best, various parameters may have been associated with marginal increases in the risk of developing one disorder or another, but under such conditions that they do not allow any firm conclusions. They are therefore of little interest to practitioners or patients.
Thus, despite decades of intensive research :
- No marker or biological test has been validated to contribute to the diagnosis of mental disorders;
- No new class of psychotropic drugs has been discovered in the last 50 years, so much so that the pharmaceutical industry has virtually ceased research in this area since 2010. The current drugs were discovered in the 1950s-1970s by serendipity1, or are derivatives obtained by trying to reduce their adverse effects. Their effectiveness is also considered low by the latest publications.
These results are now supported by such a large body of work that the idea of continuing with the same neurobiological hypotheses is questionable. The likelihood of discovering a biological cause of mental disorders that would support the pharmacological approach of biological psychiatry is diminishing as studies progress.
This change of perspective began to emerge in the course of the 2000-2010s and is now widely supported by the most renowned specialists at international level.
For example, Steven Hyman, former director of the National Institute of Mental Health ((NIMH, the American institute for mental health research), states that “although neuroscience has made progress in recent decades, the difficulties are such that the search for the biological causes of mental disorders has largely failed“. Similarly, Thomas Insel, who succeeded him as head of the prestigious institute, recently admitted that “neuroscience research has, for the most part, yet to benefit patients.”, and that “the issues raised by biological psychiatry research were not the problem facing patients with serious mental illness”.
The most prestigious scientific journals are increasingly taking the same line. Psychiatrist Caleb Gardner (Cambridge) and medical anthropologist Arthur Kleinman (Harvard) wrote in the New England Journal of Medicine in 2019:
“Although the limitations of biological treatments are widely recognized by experts in the field, the prevailing message to the general public and the rest of medicine is still that the solution to mental disorders is to match the right diagnosis to the right drug. As a result, psychiatric diagnoses and psychotropic drugs proliferate under the banner of scientific medicine, even though there is no thorough biological understanding of the causes of psychiatric disorders or their treatments.”
In general, the problems posed by the biomedical approach to mental health have been well documented for a long time in numerous works by authors from multiple disciplinary fields – neurosciences, psychiatry, human sciences, history, sociology and social sciences…
Stigmatisation effects
Contrary to the good intentions of de-stigmatisation campaigns, which thought that allowing people with mental disorders to say “it’s not me, it’s my brain” would be socially and therapeutically beneficial, several international studies have shown that it increased social rejection, perceived dangerousness and pessimism about the possibility of recovery. Caregivers adhering to this view also showed less empathy towards patients. Finally, patients were also more pessimistic about their symptoms and more likely to rely on medication.
With regard more specifically to children, biomedical conceptions have undoubtedly contributed to the increase in the prescription of psychotropic drugs. At the same time, they are generally unfavourable to psychotherapeutic, educational and social practices, which have been widely documented as effective and recommended as first-line treatment.
The example of hyperactivity and depression
In support of its analysis, the HCFEA was particularly interested in the issue of Attention Deficit Hyperactivity Disorder (ADHD), which is considered to be the most common diagnosis in school-age children, and in the issue of depression, which can be understood in terms of several mental health problems in children and adolescents.
ADHD cannot therefore
be formally qualified as
a neurological disease
or disorder
No significant results for hyperactivity
Brain imaging studies published in the 1990s suggested that advances in neurobiology would soon allow diagnostic tools to be validated. Thirty years later, no test for ADHD has yet been recognised.
Hundreds of structural and functional brain imaging studies have shown differences correlated with ADHD, but none of them correspond to structural brain changes, and even less to lesions: ADHD cannot therefore be formally qualified as a neurological disease or disorder. Moreover, they are quantitatively minimal, contradictory, and of no interest from the point of view of diagnostic and therapeutic practices or health policies. Other work suggested a dopamine deficit or dysfunction of dopaminergic2 neurons as the cause of ADHD, but this perspective has been tested and refuted.
In general, the hypotheses concerning the neurological etiology of ADHD are now scientifically weak and dated.
Initial studies also suggested a strong genetic etiology3. These associations or their causal impact have been disproved. Currently, the best established and most significant genetic risk factor is the association of ADHD with an allele4 of the gene coding for the dopamine D4 receptor. According to a meta-analysis, the associated increase in risk is only 1.33. More precisely, this allele is present in 23% of children diagnosed with ADHD and only 17% of control children. This is of no clinical relevance.
A recent review of over 300 genetic studies concludes that “the results from genetic studies of ADHD are still incohérent and inconclusive”.
Depression: neither neurological nor genetic
In 2022, Joanna Moncrieff’s team of internationally recognised experts on depression and psychotropic drugs published a study that demonstrated the inconsistency of biomedical views and drug treatments for depression.
This publication, combining reviews and meta-analyses on a panel of very large numbers of patients, aimed to produce a synthesis of the main works that have studied the links between serotonin and depression over the last three decades. Their conclusion is clear: they found no convincing evidence that depression is related to lower serotonin levels or activity.
Most studies have found no evidence of reduced serotonin activity in people with depression compared to those without depression. In addition, high-quality genetic studies with good statistical power also rule out any association between genotypes associated with the serotonin system and depression.
What consequences on diagnostic and treatment practices and health policies?
In the current state of scientific knowledge, there is no established causal link between biological mechanisms, diagnosis and treatment in the field of psychiatry, a fortiori in children. A serotonin or dopamine deficiency should therefore no longer be used to support the prescription of antidepressants or psychostimulants for depression or ADHD. This is consistent with the low effectiveness of biological treatments observed.

In the same way, one should be careful about the use of diagnostic categories inherited from large nomenclatures such as the DSM, the Diagnostic and Statistical Manual of the powerful American Psychiatric Association, an international reference. In the absence of a biological etiology, the diagnostic categories described in the DSM have no scientific validity: they do not denote any identifiable natural entity that could be interpreted as a disease. The same is true for the psychiatric diagnoses in the ICD-10, the International Classification of Diseases published by the WHO
This lack of validity is manifest in the variability of diagnoses according to the age of the child, the high proportion of co-morbidities, and the heterogeneity of clinical situations that the nomenclatures do not allow to grasp in detail – all the more so because, due to their naturalistic epistemology, they were constructed to be independent of the contexts of occurrence of the disorders.
Moreover, despite its evolutions, the DSM still suffers from reliability problems: the diagnostic decisions made by two doctors about the same patient are too often different, which limits their interest. Given its scientific weakness and considering that it “had been an obstacle to research”, the NIMH, the main funder of mental health research worldwide, disassociated itself from it.
The problem is not only epistemic but also political: since the 2000s, France has relied on the idea that these diagnoses could be the basis for standardized recommendations of good practice. The result is disappointing. Thirty years of mental health policies oriented by biomedical approaches have not prevented an increase in the psychological suffering of children and adolescents, an increase in suicide rates, a chronic deficit in the supply of care, a deterioration of institutions and care and education teams, a scissor effect between the demand for and the supply of care, unbearable waiting times, a continuous increase in the consumption of psychotropic drugs…
Taking into account the advances in research also means considering the absence of convincing results as an evolution of scientific knowledge in its own right, capable of reorienting public policies and research practices.
The current model of biological psychiatry has not lived up to its promise, in part because of the narrow and misguided application of the evidence-based approach to mental medicine, which seeks to apply research data to the clinical experience of the practitioner.
While we should not necessarily hold it against those who developed and supported it, we must now take this failure into account in order to rethink approaches, policies and systems of care, education and social intervention. In this respect, the the High Council for Family, Childhood and Age report does not limit itself to documenting the malaise and the reasons for it: it proposes new approaches and details the psychotherapeutic, educational and social strategies likely to contribute to the accompaniment and care of children, as well as the support of families.
This is where research and public policy efforts must now focus.
- Serendipity: In the scientific world designates a form of intellectual availability, which makes it possible to draw rich lessons from an unexpected discovery or an error.
- Dopaminergic: which works or reacts to dopamine. Dopamine is of many which is a chemical that serves as a neurotransmitter in the brain and is involved in “motor control, attention, pleasure and motivation, sleep, memory and cognition.
- Etiology: study of the causes of diseases. By extension: All the causes of a disease.
- An allele is a variable version of the same gene, that is to say a varied form. There are usually a few alleles for each gene, but some genes have several dozen alleles.
Authors
Sébastien Ponnou Psychoanalyst, Senior Lecturer in Educational Sciences at the University of Rouen Normandy – France
Xavier Briffault Researcher in social sciences and epistemology of mental health at the Medicine, Science, Health, Mental Health, Society Research Center (CERMES3), National Center for Scientific Research (CNRS)
Disclosure statement
Sébastien Ponnou is a qualified member of the HCFEA’s Council on Childhood and Adolescence. He directs several research projects for which the CIRNEF and the University of Rouen Normandie have received funding from public organizations and mutual foundations: Interdisciplinary Research Institute for Man and Society (IRIHS), Fondation EOVI – Fondation de l’Avenir, FEDER – Région Normandie.
Xavier Briffault is, as a sociologist and epistemologist of mental health, a qualified member of the HCFEA’s Council on Childhood and Adolescence.