UNODC hosts Consultation on Treatment of Drug Use Disorders and Associated Mental Health Disorders in Prison Settings
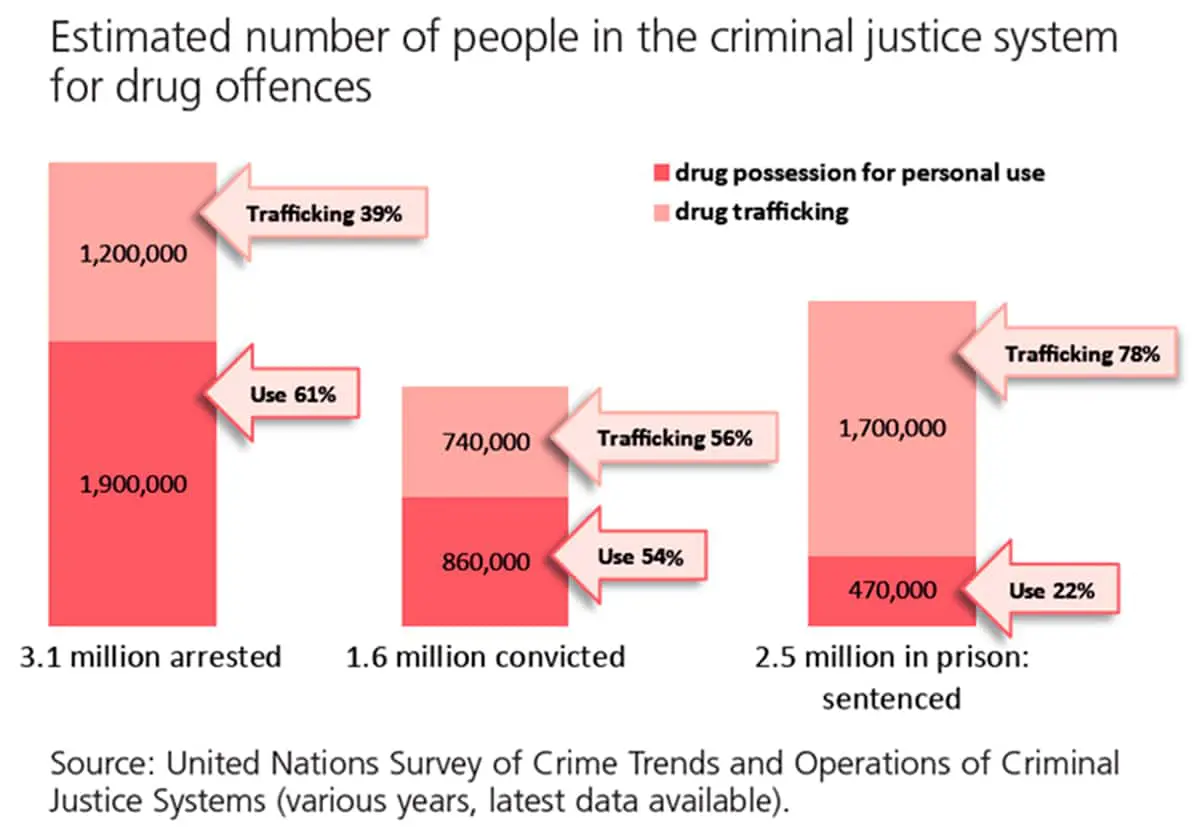
The prevalence of drug use in prison is estimated to be at 20%, around four times higher than in the general population. 22% of people in prisons are sentenced for offences related to drug possession for personal use.
In line with the International Drug Control Conventions, measures like treatment, education, after-care, rehabilitation and social reintegration can be applied as alternatives to conviction or punishment with offences involving personal drug possession.
The United Nations Office on Drugs and Crime (UNODC) and the World Health Organization (WHO) launched an initiative on “Treatment and care for people with drug use disorders in contact with the Criminal Justice System” and have published a handbook on “Alternatives to Conviction or Punishment” to support the implementation of such measures through health and justice partnerships.
Prison is a high-risk environment, exposing people in prisons to many health threats. According to the Nelson Mandela Rules, people with severe mental health disorders should not be detained but transferred to adequate health facilities. Nevertheless, epidemiological studies indicate high prevalence rates for mental health conditions (e.g. depression, suicide risk) and substance use disorders in prison settings.
Addressing drug use disorders and associated mental health disorders in prison settings
© iStockphoto/MoreISO
A UNODC informal technical consultation on addressing drug use disorders and associated mental health disorders in prison settings brought together 120 experts from 53 countries. Health and justice practitioners, researchers, policy makers, civil society, people with lived experience1, and representatives of regional and international organizations shared practices, challenges and needs on drug use and associated mental health disorders in prison settings.
Closing the overall treatment gap for people with drug use disorders and increasing the accessibility of evidence-based treatment were underlined as key efforts to reduce substance use and criminal justice contacts as well as associated prison overcrowding, thus improving public health and public safety in a synergic approach, benefitting both communities and prison settings.
Pharmacological treatments for opioid use disorders, including when offered in prison settings, are effective clinical interventions in reducing substance use, related mortality and morbidity, as well as recidivism and reincarceration. Psychosocial interventions such as cognitive behavioural therapy, contingency management, community reinforcement approach and therapeutic communities, including opioid overdose prevention trainings, were also considered beneficial.
Universal health coverage and equity are critical concepts for quality prison health service, and cooperation between health, justice and social services will ensure that people with drug use and associated mental health disorders in prisons are not left behind.
UNODC will continue to support Member States in improving prison health services and hopes to launch a project of evidence-based interventions in prison settings with an emphasis on low- and middle-income countries.







